Neurosurgery service provides care for patients with the nervous system disorder of the brain, spine, nerve and muscle. Service include screening, diagnostic, curative and palliative care.
The aims of this specialized unit are:
- To provide comprehensive and high-quality clinical care at subspecialty level to neurosurgical patients in the country.
- To provide excellent training for clinical neuroscience specialists; allied health professional and basic neuroscientists.
- To conduct high-quality neuroscience research involving experts from different disciplines.
- To serve as the centre of excellence in clinical neurosciences in the South East Asia region.
- Skull Base Surgery
- Paediatric Neurosurgery
-
Functional Neurosurgery
(Movement Disorder) - Epilepsy Surgery
- Neuro-Oncology
- Spine Surgery
- Neurovascular Surgery
- Pain & Interventional
- Radio Surgery
There can be various problems that can occur within the spinal column, cord or the nerves that could affect the smooth function of this amazing structure. The problems could range from minor “wear and tear” known as degenerative conditions to more sinister conditions such as tumours. The other condition that could affect the spine includes infection, disc prolapses, traumatic fractures, osteoporotic fractures, vascular malformation and developmental problems such as spinal lipoma and tethered cord syndrome.
These problems need to be evaluated clinically by taking a good history and complete physical examination. Then the relevant investigations need to be conducted eg. X rays, CT scan, MRI scans, nerve conduction studies etc. The MRI images are of high resolution (1.5 to 3.0 Tesla). Once the exact problem has been identified, the management strategy is formulated that is suitable to that particular patient considering all factors eg. age, medical background, degree of disability etc.
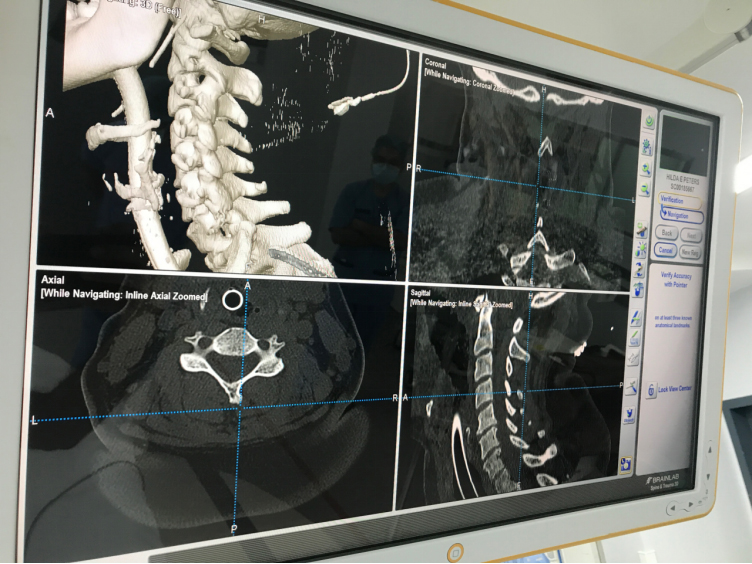
The surgical treatment is varied depending on the condition. It is carried out in operation theatre mostly under general anaesthesia. The “state of the art” equipments are available at our disposal and are used for the cases in order to obtain the best possible outcome. The equipment available to be used includes high end microscope, BRAINLAB image guidance system, intraoperative neurophysiological nerve monitoring, endoscopes, ultrasonic aspirators etc.
Post operative recuperation is managed with adequate analgesia eg oral analgesic, patient controlled analgesic (PCA) etc. Few days after surgery, physiotherapy and rehabilitation therapy is instituted.
There are host of paediatric neurosurgical problems that can affect a newborn, infant, toddler, teenager and adolescence. When the baby is born with a particular condition is known as a congenital condition. However, if the baby is born normal but over the years develop a condition it is an acquired or developmental condition.
Paediatric neurosurgical services would admit children between the ages of a newborn up to the age of 18 years old. The conditions that affect children vary with the age group which may involve the brain or the spinal cord.
The newborn may have congenital conditions example protrusion of a sac or brain from the defected skull or spine, abnormal lumps, dimples or hairy patches at the lower back, enlarging head circumference, abnormal skull shape etc. These various conditions of meningoencephalocele, spinal lipoma, hydrocephalus, tumours and craniofacial syndromes need urgent neurosurgical attention.
The older child may develop progressive unsteadiness on the feet, seizure, weakness, blurring of vision, persistent vomiting etc. These are symptoms of a possible brain or spinal cord problem eg. brain tumours, spine tumours, abnormalities in the spine formation etc. These problems need to be evaluated clinically by taking a good history and complete physical examination. Then the relevant investigations need to be conducted eg. X-rays, Ultrasound scans, MRI scans, nerve conduction studies etc. The MRI images are of high resolution (1.5 to 3.0 Tesla). Once the exact problem has been identified, the management strategy is formulated that is suitable to that particular patient considering all factors eg. age, bone maturity, and weight of the child etc.
The common conditions treated in the unit range from congenital problems of brain and spine eg. meningoencephalocele, spinal lipoma etc; developmental problems etc. craniocervical problems; brain tumours; spinal tumours; hydrocephalus; craniosynostosis (non-syndromic and syndromic) and traumatic brain and spinal injury.
There is a multidisciplinary team to deal with craniofacial cases which compose of neurosurgeons, maxillofacial surgeons, ENT surgeons, eye surgeons, geneticist, paediatric intensivist, paediatric anaesthetist, physiotherapist, social worker etc.
The surgical treatment is varied depending on the condition. It is carried out in operation theatre mostly under general anaesthesia. The “state of the art” equipments are available at our disposal and are used for the cases in order to obtain the best possible outcome. The equipment available to be used includes high-end ZEISS microscope, electromagnetic MEDTRONIC AXIEM S7 image guidance system, neurophysiological intraoperative nerve monitoring, endoscopes, ultrasonic aspirators etc.
The post-operative care is carried out in the intensive care unit or high dependency unit depending on the condition. The brain and spinal tumour cases are jointly managed with the paediatric oncologist.
The patients are followed up in the clinic periodically to assess their clinical condition and well being. Some patients would also require serial imaging eg MRI scans.
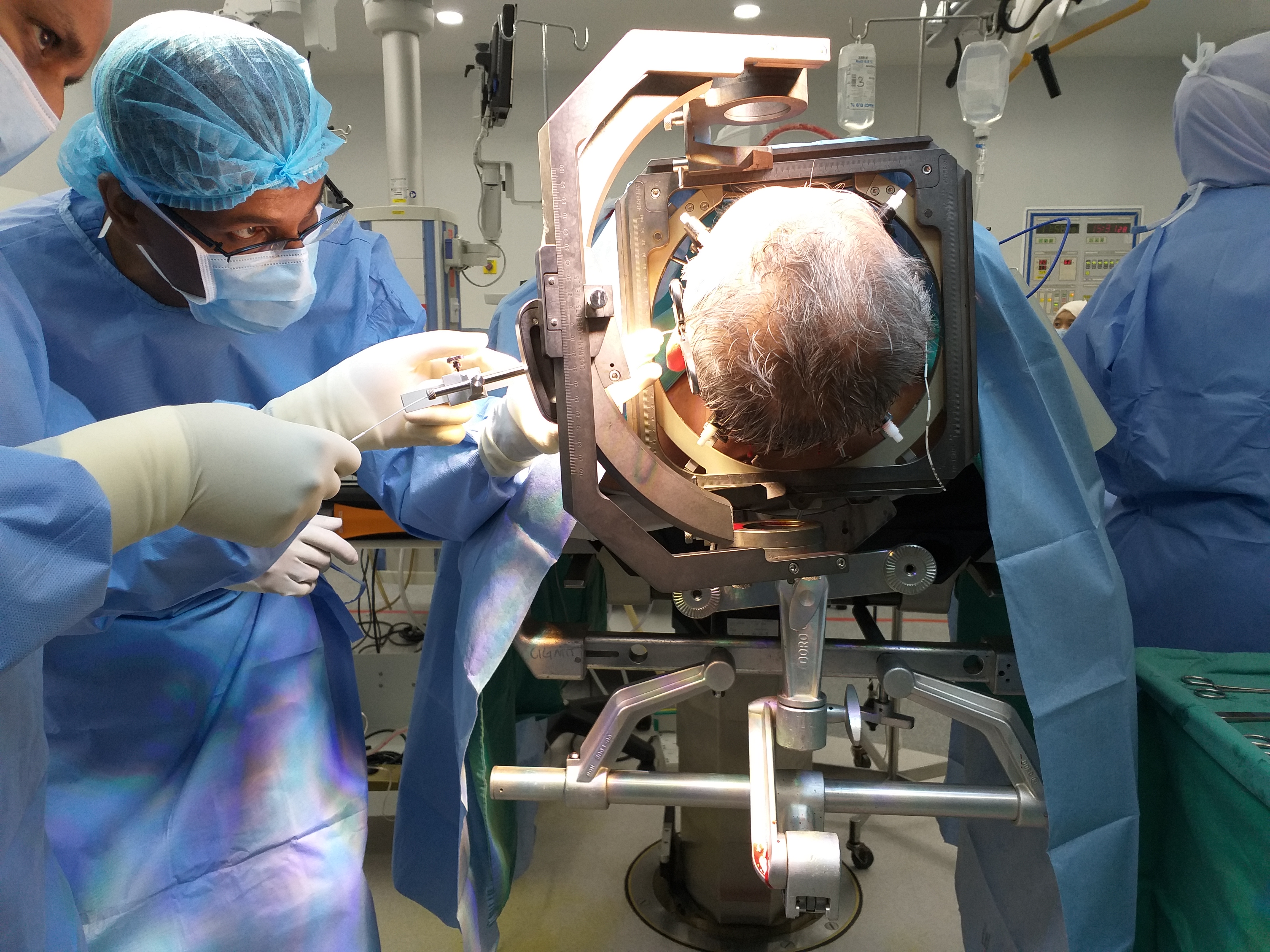
The Functional Neurosurgery Service of UMMC & UMSC offers surgical treatments such as Deep Brain Stimulation (DBS) for movement disorders and other related conditions.
The service also offers a full range of stereotactic procedures including lesioning.
Examples of conditions treated include Parkinson’s disease, tremulous disorders and dystonic conditions as well as other more unusual movement disorders. The group runs inter-specialty joint clinic consultations involving neurosurgery and neurology for patients with complex movement disorders referred for DBS surgery.
The goal of epilepsy treatment is to reduce/stop seizures and improve the quality of life in our patients. As such, patients with refractory /uncontrolled epilepsy are prime candidates for assessment of suitability for surgical management.
In University Malaya Medical Centre, these patients are reviewed by a dedicated group of doctors with special interest in Epilepsy. This includes adult and paediatric epileptologists / neurologists, Epilepsy surgeons, Neuroradiologists, Psychologists and skilled electrophysiology technicians.
Being a premier academic setting allows us to provide the highest standard of treatment while paving the way advanced research and clinical care for the benefit of patients seeking treatment in our hospital. We aspire to tailor each consultation and management plan to the individual needs of our patients while at the same time adhering to International guidelines and best available evidence.
- Each individual case is initially seen and assessed by the Neurologist in a dedicated Epilepsy Clinic to determine intractability to medication and suitability for surgical assessment
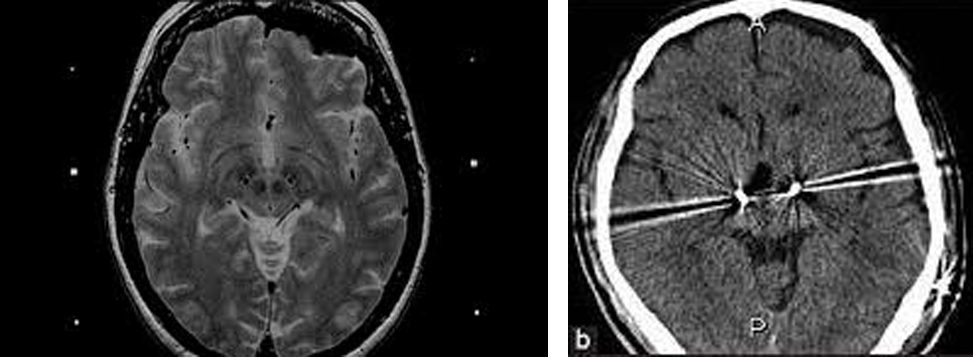
- Patients undergo multiple assessments – primarily clinical, radiological (MRI, PET, SPECT) and electrophysiological (24 hour VEM) to determine suitability for surgery
- Every individual case is discussed in our Epilepsy MDT to assess for suitability for surgery
- Once surgical suitability is established, the patient will be seen in our Neurosurgery outpatient clinic to discuss surgical options and admission/ surgical procedure including risk and benefits of the procedure
- Patient undergoes surgery
- Patient is followed up in the Neurosurgery and Neurology clinics.
Our Comprehensive facilities include:
- Brain suite supported Intra operative Image guidance
- Intra operative MRI
- Intra operative Neurophysiology monitoring
- Awake Surgery services
- Frame Based Stereotactic surgery
- Advanced Imaging services
- 3T MRI
- Diffusion weighted imaging
- MR Spectroscopy
- Functional MRI (fMRI)
- Ictal SPECT Scan
- PET Scan
- WADA test
- DTI mapping
- 24 hour video telemetry (Video EEG)
- Epilepsy Source imaging
- Frame based SEEG monitoring
- Depth and Strip electrode insertion
- Intra operative Brain mapping
Among the surgery performed include :
- selective amygdalohipocampectomy
- anteromedial temporal lobectomy
- resection of focal cortical dysplasia (FCD)
- resection of low grade tumors
- Corpus callosotomy
- Endoscopic Hemispherotomy
- Vagal nerve stimulator (VNS) insertions.

- Primary Brain Tumors
- Benign Brain Tumors
- Meningioma
- Craniopharyngioma
- Malignant Brain Tumors
- Low grade Glioma
- High Grade Glioma
- Medullobalstoma
- Secondary Brain Tumors(Metastatic Brain Tumor)
- Pituitary tumor
- Skull Base tumour
- Spinal Tumors
- Intramedullary tumors
- Intradural Extramedullary tumos
- Metastatic Spinal Tumors
- Benign Brain Tumors
- Each individual case is seen initially in our outpatient clinic or as emergency admission in the ward by a Consultant Neurosurgeon.
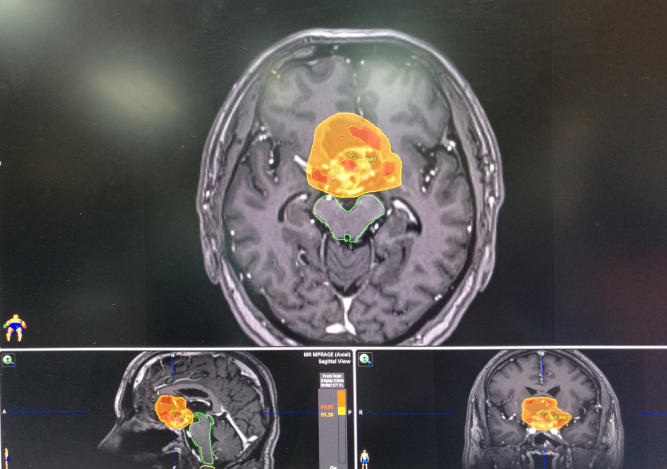
- All relevant investigations including MRI Brain is performed.
- The patient’s clinical and radiological findings is then discussed in a multidisciplinary meeting to decide on the best course of action
- Patient undergoes surgery
- The histopathology report and post-surgery imaging is discussed in the multidisciplinary meeting to ensure optimal adjuvant therapy based on the latest evidence
- Patient undergoes adjuvant therapy under the care of oncologists
- Patient is followed up in the Neurosurgery and Oncology clinics
- Dedicated subspecialised neurosurgeons
- Neuro Oncology Surgeon
- Paediatric Neurosurgeon
- Radiosurgeon
- Advanced Equipment
- Brain suite supported Intra operative Image guidance
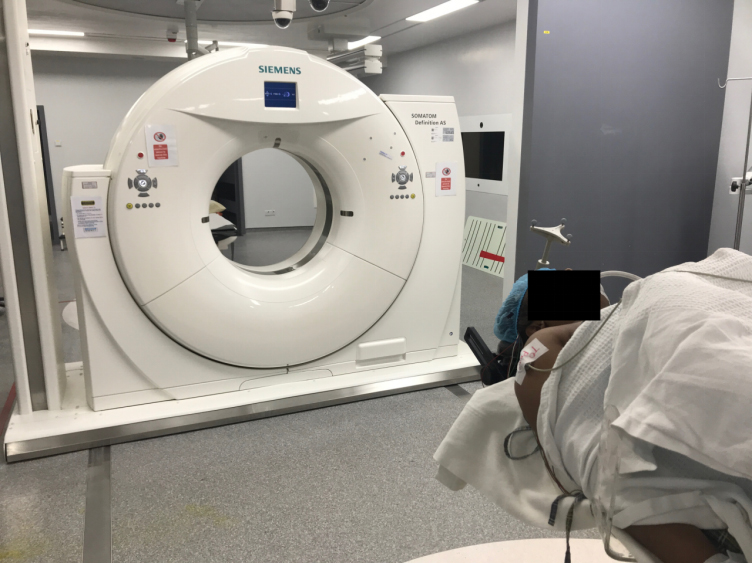
- Intra operative MRI
- Intra operative CT
- Intra operative Neurophysiology monitoring
- Awake Surgery services
- Frame Based Stereotactic surgery
- 5ALA fluorescence guided surgery
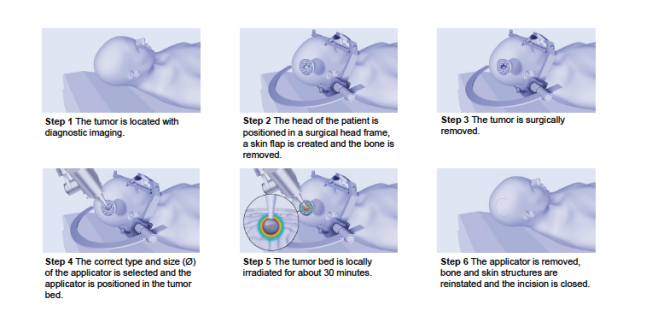
- Intra operative Radiotherapy (IORT)
- Advanced Imaging services
- 3T MRI
- Diffusion weighted imaging
- MR Spectroscopy
- Functional MRI (fMRI)
- SPECT scan
- PET Scan
- Dedicated Neuro Oncology Services
- Chemotherapy
- Radiotherapy
- Stereotactic radiosurgery via LINAC Linear Accelerator
- Stereotactic radiotherapy (SRT)
- Intensity modulated radiotherapy (IMRT
Symptoms of Brain tumor depend on the type, site, size and patients own co morbidities.
Common symptoms include:
- Headaches – persistent over a period of time; usually worse in the mornings
- Nausea and vomiting
- Confusion
- Seizures
- Focal seizures – involving recurrent jerking movement of one part of the body
- Generalized seizures – involving the whole body
- either a sudden cessation of all movement or
- a significant jerking of the whole body
- Personality and memory changes
- Depression, loss of interest, loss of inhibition, mood changes
- Short term or long-term memory impairment
- Fatigue
- Sleep problems – unable to sleep or sleeping too much
- Weakness of one side of the body – similar to a mild stroke
- Loss of balance and difficulty in walking
- Slurring of speech
- Acute blurring of vision
- Acute loss of hearing
- Blood tests
- Radiological investigations
- CT Brain – usually the first imaging investigation
- MRI Brain – with advanced sequences
- If you could be pregnant
- What drugs you are taking including supplements, vitamins, or herbs
- If you have been drinking a lot of alcohol
- If you take aspirin or anti-inflammatory drugs such as ibuprofen
- If you have allergies or reactions to medications or iodine
- Ask your doctor which drugs you should still take on the day of the surgery.
- Always try to stop smoking.
- You may have a bladder catheter inserted for monitoring purposes
- You may have blood transfusion given if blood loss is significant
Surgery will involve
- Anesthesia – usually General Anesthesia
- Shaving of part of the scalp
- An incision on the scalp
- Removal of part of the bone flap, the size dependent on the pathology
- Removal of tumor
- An intra operative MRI (if necessary)
- Re-fixation of bone flap with titanium screws and plate
- Closure of scalp wound
- In Awake Surgery– the patient is usually awake for part or the whole surgery. The preparation for these patients includes pre op introduction to the operating team, the operating environment, the tests to be performed during surgery and intraoperative neurological assessment while patient is awake
- The patient will be given a scalp block (Regional anesthesia) during surgery to reduce the sensation in the surgical site
Risks for any anesthesia are:
- Reactions to medications
- Problems breathing
Possible risks of brain surgery are:
- Surgery on any one area may cause problems with speech, memory, muscle weakness, balance, vision, coordination, and other functions. These problems may last a short while or they may be permanent
- Blood clot or bleeding in the brain
- Seizures
- Stroke
- Coma
- Infection in the brain, in the wound, or in the skull
- Brain swelling
- You will be monitored in the Neuro Intensive Care Unit (NICU) or the High Dependency Unit (HDU)
- You may be allowed some fluid and soft diet as decided by the surgeon
- You may have an intravenous drip, a bladder catheter as well as drains from the wound site
- In some cases, you may have a feeding tube inserted via the nose/mouth to aid with the feeding while you recover
- The post-operative pain is usually controlled with intravenous, intramuscular or oral medication
- In most cases, the patient is expected to walk by the second day of surgery
- Your stay in the hospital may range from 3 days to much longer depending on the severity of the disease and associated factors
- You may need physical therapy (rehabilitation) post-surgery to improve mobilization
- Once discharged, you will be given advice on home care including wound care, diet and exercise
- The histopathology report usually takes between 7 to 14 days to be ready, depending on the complexity of the case
- Once the report is ready, the case is discussed in the multidisciplinary meeting to decide on the best options of management post operatively
- You will be seen in the Surgical outpatient clinic between 7 to 14 days post-surgery
- During this visit, the wound stitches (if any), will be removed
- Your wound will be inspected for healing
- You will then be informed of your tumor histopathology report and adjuvant therapy including chemotherapy, radiotherapy or radiosurgery
- In some cases, you will only need ot be followed up with regular MRI scans to ensure no recurrence of tumor happens
- You may have to continue with physiotherapy to improve any post-operative neurological weakness
The UM Neuro Oncology team is actively involved in a number of different types of research involving neuro oncology management. Our work includes pre-clinical laboratory research and translational research, as well as interventional and observational clinical trials. We hope to identify better ways to diagnose, prognosticate and follow up our patients with brain tumors. We also look at optimising treatment in this group of patients to improve their quality of life as well as life expectancy.
- Spine Trauma – including Vertebral Column Fractures and Spinal Cord Injury involving the Cervical, Thoracic and Lumbar Segments of the construct.
- Degenerative Conditions entailing Decompression with or without Stabilization with Instrumented Fusion:
-
- Low back pain (lumbago), sciatica,radiculopathy and neurogenic claudication from lumbar canal stenosis.
- Cervicalgia (neck pain), brachialgia,radiculopathy and myelopathy from cervical canal stenosis.
- Intervertebral disc herniation – discectomy, discectomy & fusion, and Discectomt & artificial disc replacement.
- Craniocervial Junction, Upper Cervical Spine and Subaxial abnormalities from anomalies of development, degeneration and disease with resultant instability requiring Decompression & Stabilization
- Spinal Cord Tumours
-
- Primary Spinal Cord Tumours (Intramedullary Spinal Cord Tumours) including ependymomas, astrocytoma and haemangioblastomas
- Secondary spinal cord tumours – metastatic spinal cord tumours, Extradural & Intradural.
- Nerve sheath tumours (Intradural Extramedullary)– neurofibroma/schwannoma
- Congenital conditions
-
- Spina bifida
- Chiari Malformation
- Vascular Spinal Lesions – vascular malformations/cavernomas
- The Management of Syringomyelia
- Aneurysms
- Arteriovenous malformations (AVMs)
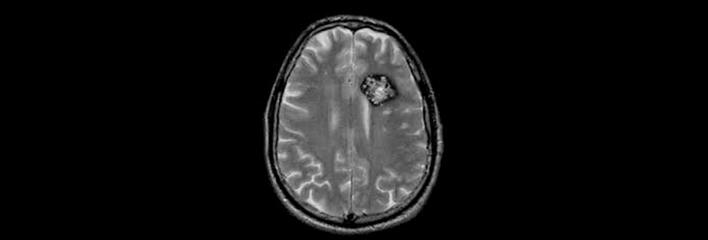
- Cavernous malformation
- Dural arteriovenous fistula
- Moyamoya disease
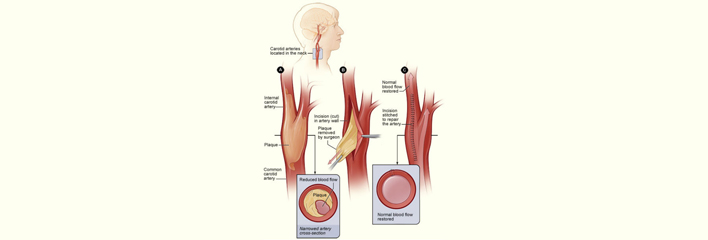
- Carotid artery disease (CAD)
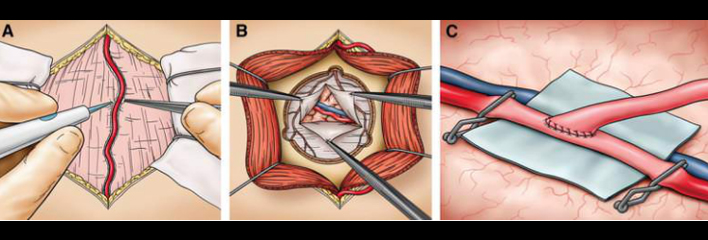
I. Surgical Intervention
Intracranial aneurysm, also known as brain aneurysm, is a cerebrovascular disorder in which weakness in the wall of a cerebral artery causes a localized dilation or ballooning of the blood vessel. They can be located in the anterior or posterior circulation. Aneurysms in the posterior circulation (basilar artery, vertebral arteries and posterior communicating artery) have a higher risk of rupture.
The management of ruptured cerebral aneurysms is a clinical emergency involves urgent surgical or neuroradiological intervention
- Arteriovenous Malformations (AVM) – intracranial arteriovenous malformations (AVMs) are abnormal connections between the arteries and veins in the brain. M Most people with brain or spinal AVMs experience few, if any, major symptoms. About 12 percent of people with this condition experience symptoms that vary greatly in severity.
- Angiographically Occult Vascular Malformation (AOVMs):
- Cavernomas – Cavernous hemangioma, also called cavernous angioma, cavernoma, or cerebral cavernoma is a type of benign vascular tumor or hemangioma, where a collection of dilated blood vessels form a lesion. Because of this, blood flow through the cavities, or caverns, is slow. Additionally, the cells that form the vessels do not form the necessary junctions with surrounding cells. Also, the structural support from the smooth muscle is hindered, causing leakage into the surrounding tissue. It is the leakage of blood, known as a hemorrhage, from these vessels that causes a variety of symptoms known to be associated with this disease.
- Dural AVMs – A dural arteriovenous fistula or Malformation, is an abnormal direct connection between a meningeal artery and a meningeal vein or dural venous sinus.
- Carotid-cavernous fistula – Usually a consequence of trauma.
- Hemangioblastomas – Hemangioblastomas are vascular tumors of the central nervous system that originate from the vascular system, usually during middle age. Sometimes, these tumors occur in other sites such as the spinal cord and retina. They may be associated with other diseases such as polycythemia, pancreatic cysts and Von Hippel–Lindau syndrome. Hemangioblastomas are most commonly composed of stromal cells in small blood vessels and usually occur in the cerebellum, brainstem or spinal cord. They are classed as grade I tumors under the World Health Organization’s classification system.
- Spinal Vascular Malformations
- Cerebral arterial dissections
- Atherosclerotic cerebro-vascular disease
- Cerebrovascular venous thrombosis
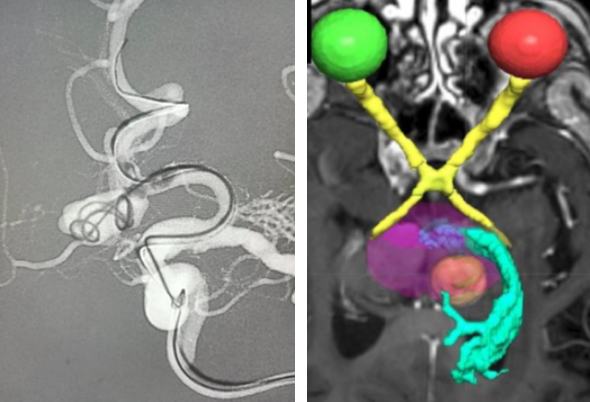
- Moyamoya Disease – Moyamoya disease is a disease in which certain arteries in the brain are constricted. Blood flow is blocked by constriction and blood clots. A collateral circulation develops around the blocked vessels to compensate for the blockage, but the collateral vessels are small, weak, and prone to bleeding, aneurysm and thrombosis.
Involving both the paediatric and adult population.
Management Options:
The surgical management includes:
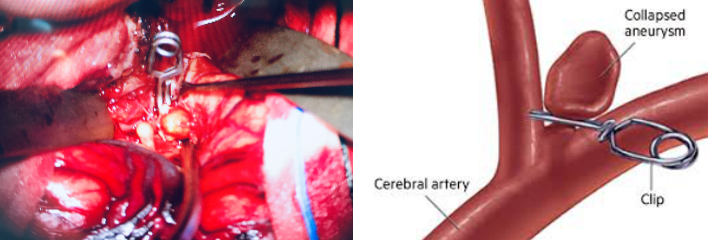
Surgical clipping of aneurysms to exclude it from the circulation
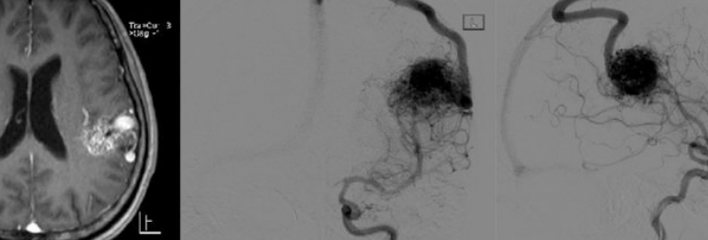
Surgical excision of AVM niduses to reestablish non-communication in the arterio-venous trees
Cavernoma and hemangioblastoma excision surgery.
II. Interventional Neuroradiology
We work closely with Interventional Neuroradiologists who offer the option of non-surgical Radiological intervention services as an alternative to Surgery for aneurysms and AVMs and Carotid Artery Stenosis where indicated. All cases are appraised by a Multidisciplinary Team of Neurosurgeons and Interventional Neuroradiologist as to the most appropriate treatment of the same pertaining to that case.
The UMMC & UMSC Radiosurgery Services includes leading Neurosurgeons, Neuro-oncologists, Radiation Oncologists, Neuropathologists and Rehabilitation Physicians and Technical & Paramedical Support Staff. This Multidisciplinary Team delivers sophisticated care and uses up to date technologies to treat patients with Neoplasms of the Brain, Spine and Skull Base.
Utilising the Novalis Tx Radiosurgery systems with state-of-the-art technology that integrates treatment planning in one system. A one of a kind technology that can treat both non-cancerous and cancerous conditions in a very less time is known as Novalis Tx radiosurgery system. Novalis radiosurgery accurately shapes the radiation beam to the area to be treated and uses imaging guidance and other methods to target the tissue or tumor to be treated while avoiding surrounding healthy tissues. Stereotactic radiosurgery is a non-invasive process that delivers high doses of radiation on the tumor from different angles.
Novalis Tx is an ideal technology for treating those tumors that were previously located in inaccessible locations and were difficult to treat. This technology decreases the treatment time as the high-dose radiation beams matches the shape of the tumor that is being treated. The potential errors are also reduced as in the case of time consuming procedures. The entire treatment session can be completed in just 15 minutes.
Applications:
- Neuro-oncology – Brain (Extra-axial and Metastatic Tumours) and Spine (Intradural- Extramedullary & Intramedullary).
- Vascular Neurosurgery – management of inoperable or eloquently located arterio-venous malformations and angiographically occult vascular malformations.
- Craniofacial Pain Syndromes – In the Management of Trigeminal Neuralgia, and other Cephalic Neuralgias.
- Skull Base Neurosurgery – As a Primary and Secondary Treatment Modality in management of cerebellopontine angle tumours, petrosal tumours, sellar lesions and paragangliomas.
- Pituitary Tumours & Craniopharyngiomas.
- Other Applications – Novalis Tx radiation therapy has also applications in thetreatment Seizures, Parkinson’s disease, Obsessive Compulsive Disorder and Cluster Headaches.
Application in Neuro-oncology
While surgery generally but not invariably remains the primary and definitive management in neuro-oncology, in both Primary and Stereotactic Radiation Therapy, both Stereotactic Radiosurgery (SRS) and Stereotactic Radiotherapy (SRT) are increasingly becoming an adjunct tool in the management of the same and increasingly replacing surgery as the primary modality of treatment.
The utility and indications of SRS and SRT in our Centres is Evidence Based
Since the launch of Radiosurgery Services at UMMC in 2015, Stereotactic Radiation Therapy is only selectively not given to excised tumour beds in cerebral metastasis, where in radiation therapy is not the primary management.
Stereotactic Radiosurgery is also used as adjuvant therapy in the management of Benign Tumours of higher grades viz Atypical Meningiomas.
Application in Vascular Neurosurgery
The Spetzler-Martin Classification is an arbitrary system that stratifies the complexity of arteriovenous malformations (AVMs) with regards to surgery based on their size, eloquence of location and the veins the malformations drain into.
Before the advent of stereotactic radiation therapy, high grade AVMs where either managed expectantly, or were associated with significant surgical morbidity. With the evolution of Stereotactic Radiation Therapy, high grade complex AVMs have been treated successfully through single treatments, the application of fractionations or the staging of treatment utilizing both applications.
The management of brainstem and thalamic angiographically occult vascular malformations namely Cavernomas with stereotactic radiation therapy to decrease the incidence and frequency of haemorrhages, has become evidence-based.
Application in Craniofacial Pain Syndromes.
Craniofacial Pain Syndrome is increasingly becoming prevalent in our population. When there is an absolute or relative contraindication for Surgical Microvascular Decompression, Stereotactic Radiosurgery is increasingly being utilized ahead of more invasive techniques such as percutaneous trigeminal rhizotomy – radiofrequency ablation and glycerol injections
Application in skull base surgery
In UMMC & UMSC, virtually all Vestibular Schwannomas (Acoustic Neuromas) less then 3cm in size with hearing impairment and no brainstem compression have been treated successfully with stereotactic radiosurgery. A definite treatment algorithm exists for treatment of larger lesions with Microsurgery or Hyperfractionated Stereotactic Radiosurgery.
A series of Paragangliomas mainly Glomus Tympanicum and Glomus Jugularae have been treated successfully as the primary modality of treatment at our Centres since 2015.
Stereotactic radiation therapy is also rapidly becoming a treatment modality for pituitary tumours and Craniopharyngiomas. In our Centres, Radiosurgery is employed when Surgical and Medical Therapies fail to achieve Biochemical Cures in conditions of Functioning Pituitary Adenomas namely, Acromegaly, Cushings’ Disease and Prolactinomas.
Craniopharyngiomas though histologically benign, are tumours composing of solid and cystic component that arise from the pituitary stalk. They are difficult to cure, making them malignant in behavior. A series of residual and recurrent Craniopharyngiomas following surgery treated with Radiosurgery at our Centres have shown good control of the cystic and solid components of these residual /recurrent tumours.
 |
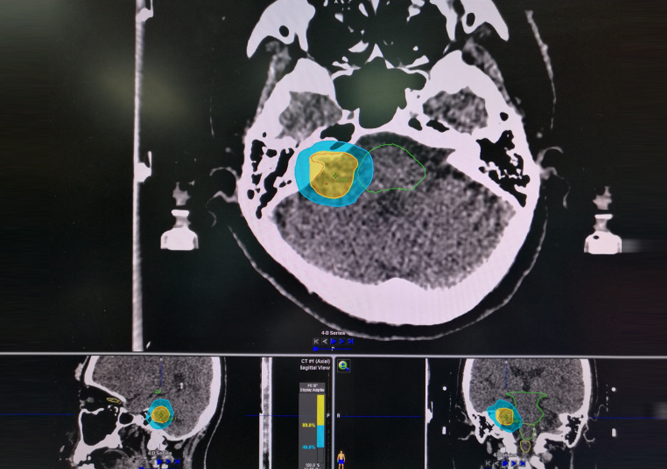 |
- Intraoperative radiation therapy (IORT) is an intensive radiation treatment that’s administered during surgery. IORT allows direct radiation to the target area while sparing normal surrounding tissue. In UMMC & UMSC IORT is used to Brain Metastases where there is a concern that microscopic amounts of cancer may remain.
- A miniature and mobile X-ray source which emits low energy X-ray radiation in isotropic distribution. Due to the higher ionization density caused by soft X-ray radiation in the tissue, the relative biological effectiveness of this low-energy X-rays on tumour cells is higher when compared to high-energy X-rays or gamma rays.
-
In the future we are aiming to be able to provide this emerging technique to treat primary and metastatic brain tumors that can be hard to reach with conventional surgery.
LITT is performed by implanting a laser catheter into the tumor and heating it to temperatures high enough to kill the tumor, while HIFU is a non-invasive therapeutic technique that uses non-ionizing ultrasonic waves to heat tissue and ablate the lesion.
NEUROSURGERY CLINIC CONSULTATION
| Day | Time | Activity |
| Monday | 8-9am | Neuro Radiology Multidisciplinary meeting |
| 10-12pm | Chronic Pain Intervention Clinic Menara Selatan | |
| 2-5pm | Neurosurgery Outpatient Clinic Tingkat 1, Menara Utama Pusat Perubatan Universiti Malaya | |
| Tuesday | 8-5pm | Neurosurgical Operating Schedule |
| Wednesday | 8-9am | Neuro Oncology Multidisciplinary meeting |
| 8-5pm | Neurosurgical Operating Schedule | |
| Thursday | 8-9am | Epilepsy Surgery Multidisciplinary meeting |
| 9-12pm | Radiosurgery Clinic | |
| 8-5pm | Neurosurgical Operating Schedule | |
| Friday | 8-5pm | Neurosurgical Operating Schedule |